Two cases of intraventricular hemorrhage evacuation by open craniotomy assisted with stereotaxy, leading to excellent resultsKeywords: outcome, stereotactic assisted, craniotomy, Glasgow Coma Score (GCS), Intraventricular HematomaInteractive ManuscriptAsk Questions of this Manuscript: What is the background behind your study?This is a case report of two patients who presented with hypertensive intraventricular hematomas. What is the purpose of your study?This question was not answered by the author Describe what you did.Stereotaxy assisted craniotomy was used to evacuate the intraventricular hematoma. The intervention was carried out within 24 hours of the onset of the hemorrhage. Describe your patient group.This question was not answered by the author Describe your main findings.Patients recovered without any residual neurological deficit. Describe the main limitation of this study.This question was not answered by the author Describe your main conclusion.We conclude that even at a low Glasgow Coma Score of 6, an early intervention within 24 hours may lead to an excellent out come in hypertensive unilateral intraventricular hemorrhage, where the ICH is small. A conventional craniotomy might be helpful in certain cases. Describe the importance of your findings and how they can be used by others.Comparison of this concept to simple external ventricular drainage of the hemorrhage is warranted. What is the background of your topic?An intraventricular hematoma (IVH) that is extending from a hypertensive intracerebral hematoma (ICH) worsens the outcome of the patient. A low Glasgow Coma Score (GCS) on admission also relates to a poor result. Therefore, a patient who has hypertensive ICH with an IVH extension and low GCS is considered a bad surgical candidate and the neurosurgeons are reluctant to offer any major surgical intervention. Therefore, most surgeons limit the intervention to placement of external ventricular drains (EVD). These can be placed unilateral or bilateral. Whenever possible fibrinolytic agents are introduced via the EVD to expedite the clot evacuation. Generally this method will take at least a few days to remove an IVH. What is the importance to the reader/community?These two case presentations will illustrate how the IVHs of two patients (with GCS 6) were evacuated by craniotomy assisted by stereotaxy. The end result was excellent with a GCS 15 and without any neurological deficit. What is your hypothesis? (What question(s) did you ask?)This case report is published for record purposes. It may be that we are over looking a patient population who are with minimal parenchymal bleeding and an IVH extension limited to ipsilateral ventricle. Although their starting GCS is low we might be able to help them with a good outcome. What was done in your study?This question was not answered by the author What are the main conclusions derived from prior reports?This question was not answered by the author What are the main limitations of your research method?This question was not answered by the author If your work has Institution Review Board or any other supervisory authority approval, state that now: The Institutional Review Board approval was obtained for this case study. State the source of funding for this study. This study did not have any external funding.
Describe patient age (mean, range)Case 1: A left handed 40 years old hypertensive male, who has defaulted treatment for three months, was found unconscious in his bed by the housekeeper one morning. Since he was living alone the exact time of the onset of events could not be assessed. However, considering the fact that he was talking to a friend around 12 midnight, an eight hour time period was reasonable.
Emergency Room Findings: On arrival in the ER, he was breathing spontaneously and had a blood pressure of 210/120. Pupils were 3/3 (slow reacting on left side). His GCS was 6 (E-1, V-1, M-4). There was a right sided hemiparesis. The initial CT scan carried out in the ER demonstrated a significant IVH involving left frontal, temporal and occipital horns with an obstructive hydrocephalus. A small ICH was observed in the left thalamus indicating that this might be the starting point. Describe patient sex (number male and number female)Initial Procedure and Observation: Bifrontal External Ventricular Drains (EVD) were placed immediately. The Right EVD had an opening pressure above 40cm and the cerebrospinal fluid (CSF) was clear. On the left side a few drops of fresh blood was the only yield. Post procedure CT scan confirmed accurate placement of catheters, but now with a slight midline shift to the right. Within the next two hours the GCS slowly improved to 10 (E-3, V-2, M-5). But, this did not last for more than eight hours and dropped to 6 again. No fibrinolytic agents were available. Therefore, at this point (within 24hours from the initial bleed) a more aggressive intervention was planned. Describe other important patient features (symptoms (list); clinical presentation features, prior treatment, employment, etc)Surgical Planning: Since the imaging showed signs consistent with increased intracranial pressure from the initial scan, it was decided that a decompressive craniectomy should accompany any other procedure. This time a CT scan was performed with stealth protocol and a stereotaxy assisted procedure was planned. As the patient was left handed, operating on the ipsilateral brain could be considered relatively safe although this is not always true. The target was the occipital horn. It was felt that removal of a well formed hematoma from the all three horns (frontal, temporal, occipital) of the lateral ventricle would be easier from this location. Therefore, a cortical entry site was selected roughly over the parieto-occipital junction. The trajectory was about 45 degrees to the horizontal plane. Describe disease features (example = tumor subtypes) Describe the clinical intervention (ie. medications, devices, techniques) Operative Details: The left frontal EVD was removed and its entry site was incorporated to the skin incision and to the margin of the bone flap. A left sided wide fronto-temporo-parietal skin flap and a craniotomy flap covering a similar extent was made. The dura was tight; it was opened in a cruciate manner. Then the brain bulged about 1 cm in to the opening. Allowance was made for this change in the trajectory. A 1.5 cm cortical window was made at the calculated entry point. A tunnel of same diameter was dissected down to the target under stealth guidance, using only the suction cannula and the bipolar cautery. On entering the occipital horn there was a gush of CSF under enormous pressure (this indicated that the CSF in the left occipital horn and the temporal horn was entrapped by the hematoma mass that occupied the frontal horn and was not relieved by the standard placement of the EVD in the frontal horn). Then the attention was directed to remove the well formed IVH. Plain suction did not help the evacuation initially. Therefore, a small tumor holding forceps was used to crush the hematoma and these small pieces were sucked out. Later even some large clots could be easily pulled out, too. As anticipated it was much easier to pull out a temporal horn and a frontal horn clot from a occipital horn location. Once the clots were removed an inspection of the lateral ventricle was attempted. With gentle, slightly outward traction using a malleable soft retractor one could visualize most of the temporal horn through the entry tunnel. This confirmed that the temporal horn was clear of any clots. For the frontal horn, same visualization was not possible beyond the upper surface of the thalamus. Although the microscope was on stand-by the need for its use never arose. As soon as the CSF and the IVH was removed the brain sank in to the cranial cavity making the bone flap exclusion highly unnecessary. A ventricular catheter was introduced through the cortical opening to the occipital horn and was directed to the temporal horn and was left at that location. The dural flaps were brought back to the center but was not sutured. A Duragen layer was placed on top of the dura. The bone flap was replaced. Skin and galea was closed in the usual manner. The entire surgical procedure took 98 minutes. Describe the tests used to perform your research (Imaging, Patient Outcomes, Other specific tests.) What percent of study subjects completed each of the tests?Case 2: A right handed hypertensive 63 years old male who has defaulted treatment for several months suddenly became unconscious at home around 10 pm. He was rushed to the local hospital where he was intubated and was transferred to a major neurosurgical center. The CT scan of the head revealed a significant large intracranial hematoma. Due to the low GCS it was decided that non operative management should be carried out and the extremly poor prognosis was notified to the family. The family insisted that maximum possible surgical intervention be done to the patient and the patient was transferred to our center at their request. By this time about 10 hours has elapsed from the initial event.
Emergency Room Findings: On arrival in our ER he was intubated and ventilated; had a blood pressure of 240/110. Pupils were 5(right)/3(left) (slow reacting on both sides). His GCS was 5T (E-1, V-T, M-4). There was a left sided hemiparesis. The initial CT scan which was performed in the other center demonstrated a significant IVH involving right temporal and occipital horns with an obstructive hydrocephalus. Right frontal horn did not have any blood, but was compressed. No ICH could be demonstrated. Describe who conducted the tests. (Study investigators or other parties?)Surgical Planning: This was same as the previous case. The difference was that it was on right side. Since there was no frontal horn involvement it was anticipated that the duration of the procedure would be shorter. As immediate surgical evacuation was planned no attempt was made for EVD placement. Were the tests validated for use in this kind of study?Operative Details: Right fronto-parieto-temporal skin flap was developed. Fronto-parieto-temporal free bone flap was raised. The tight dura was opened in a cruciate manner. The brain bulged in to the wound. An entry was made at the junction of parieto-occipital cortex. Using a trajectory that was around 45 degrees to the horizontal plane a 1.5 cm tunnel was carved to the right occipital horn. Again CSF emitted under high pressure. A well formed IVH was visible. It was evacuated as before. The brain collapsed to the cranial cavity at this point. At the end the right temporal horn could be visualized by the light traction method that was described in case 1. An EVD catheter was placed in the right temporal horn. The dural flaps were brought back to the original configuration, but not sutured. A Duragen layer was placed over the dura. Bone was replaced and the galea and skin was closed in the usual manner. The entire surgical procedure took 82 minutes. Describe your statistical methods or tests used Describe your study power calculation (if any)The observations in these cases were made by the treating surgeons. Describe your chosen level of statistical significanceThis question was not answered by the author Provide the results for the most important outcome of your research [i.e. Patient survival] Case 1: The patient was extubated on the first post operative day. He was GCS 13 (E-4, V-3, M-6). The right extremities demonstrated a power of grade 3 and the left grade 5. The post operative scan showed a good clearance of IVH. The left temporal EVD drained cloudy CSF for 3 days. The right frontal EVD drained cloudy CSF for 24 hours then became clear. The ICP remained below 10cm. By the 10th day the power of right extremities were grade 5. It took 18 days for the speech to be perfect. He was discharged from the hospital on the 22nd day after a follow-up CT scan  . He was GCS 15 and was neurologically intact. Six weeks after the surgery he was able to take an international flight of 10 hours duration to attend to some family business. Discuss any additional outcomes of your study [i.e. Imaging findings, Patient functional outcomes, Complications]Case 2: The patient was extubated on the first post operative day. He was GCS 15. However, the left side motor power was grade 3. The right temporal EVD drained cloudy CSF for 48 hours and then got cleared. The post operative scan that was taken prior to removal of the EVD showed satisfactory results  . Left extremity power improved to grade 5 by the 7th post operative day. On 10th day a follow-up CT scan was taken and the patient was discharged home. By the 4th week he resumed his work as a manager of a pharmaceutical store. Discuss Statistical Outcomes [i.e. Multivariate analyses]This question was not answered by the author Provide the background and reason for your work and briefly summarize important prior research.Intraventricular extension of a hypertensive ICH is recognized as a bad prognostic factor. Various criteria are developed to assess the out come in such patients   ,5 ,5  ,10 ,10 . Clinicians have been using several methods to evacuate an IVH. They included catheter drainage (with or without lytic agents) and endoscopic evacuation  ,9 ,9 . Most of these methods are associated with stereotaxy. Opening into the ventricular system through a conventional craniotomy was considered to cause more harm than good (although this method was used in ruptured aneurysms or AVMs with hematoma extension to ventricles, where primary intervention needed a craniotomy) 8. However, in almost all cases the intraventricular extension has been associated with sizable ICH. Discuss the most important findings in your study.In the two cases discussed here, the ICH component is almost negligible in the CT scan. It was the IVH that was causing the obstructive hydrocephalus and the mass effect. Therefore, evacuation of the IVH relieved those effects. And the interventions were performed within 24 hours from the initial bleed. This would have helped in minimizing and deleterious effects of the blood products which were inside the ventricle. The length of entire surgery was around one and a half hour. If fibrinolytic agents were used through an EVD it would have taken much longer to evacuate a large hematoma which is located in the a lateral ventricle. Since the brain parenchymal damage was minimal from any existing small intraparenchymal hematoma, removal of the IVH itself would have reversed the situation. The other advantage of this method was that the procedure was ready for a decompressive craniotomy (although it was not required in these two cases). Although in the first case the thalamus would have been the initial site of bleeding, this is unlikely in the second case. Since the IVH was confined to the temporal and occipital horns, one might consider a choroidal artery origin or a hippocampus origin. This is reported in the literature  . Discuss the various aspects of your work (for example, treatment-related complications, comparisons to other approaches or techniques, cost-effectiveness analysis) However, in this case scenario there was no comparison with another IVH evacuation method. There was no comparison with any GCS 6 patient who was not operated. And in these two patients the IVH was involving only a single lateral ventricle. Therefore, a structured case study which compares the above criteria is needed for further evaluation of this method. Discuss Future Work and Recommendations.This is a case report consisting of two patients who presented with hypertensive intraventricular hematomas. Despite their low GCS these patients were managed aggressively with image-guided craniotomy and evacuation of hematomas. The intervention was carried out within 24 hours of the onset of the hemorrhage. Ventricular decompression and removal of clot led to full recovery. Authors concluded that even at a low Glasgow Coma Score of 6, an intervention within 24 hours might lead to an excellent out come in hypertensive unilateral IVH, where the ICH is small. A conventional craniotomy might be helpful in certain cases. This is a case report of two patients who presented with hypertensive intraventricular hematomas. Stereotaxy assisted craniotomy was used to evacuate the intraventricular hematoma. The intervention was carried out within 24 hours of the onset of the hemorrhage. Patients recovered without any residual neurological deficit. We conclude that even at a low Glasgow Coma Score of 6, an early intervention within 24 hours may lead to an excellent out come in hypertensive unilateral intraventricular hemorrhage, where the ICH is small. A conventional craniotomy might be helpful in certain cases. Comparison of this concept to simple external ventricular drainage of the hemorrhage is warranted.
An intraventricular hematoma (IVH) that is extending from a hypertensive intracerebral hematoma (ICH) worsens the outcome of the patient. A low Glasgow Coma Score (GCS) on admission also relates to a poor result. Therefore, a patient who has hypertensive ICH with an IVH extension and low GCS is considered a bad surgical candidate and the neurosurgeons are reluctant to offer any major surgical intervention. Therefore, most surgeons limit the intervention to placement of external ventricular drains (EVD). These can be placed unilateral or bilateral. Whenever possible fibrinolytic agents are introduced via the EVD to expedite the clot evacuation. Generally this method will take at least a few days to remove an IVH. These two case presentations will illustrate how the IVHs of two patients (with GCS 6) were evacuated by craniotomy assisted by stereotaxy. The end result was excellent with a GCS 15 and without any neurological deficit. This case report is published for record purposes. It may be that we are over looking a patient population who are with minimal parenchymal bleeding and an IVH extension limited to ipsilateral ventricle. Although their starting GCS is low we might be able to help them with a good outcome. The Institutional Review Board approval was obtained for this case study. This study did not have any external funding.
Case 1: A left handed 40 years old hypertensive male, who has defaulted treatment for three months, was found unconscious in his bed by the housekeeper one morning. Since he was living alone the exact time of the onset of events could not be assessed. However, considering the fact that he was talking to a friend around 12 midnight, an eight hour time period was reasonable.
Emergency Room Findings: On arrival in the ER, he was breathing spontaneously and had a blood pressure of 210/120. Pupils were 3/3 (slow reacting on left side). His GCS was 6 (E-1, V-1, M-4). There was a right sided hemiparesis. The initial CT scan carried out in the ER demonstrated a significant IVH involving left frontal, temporal and occipital horns with an obstructive hydrocephalus. A small ICH was observed in the left thalamus indicating that this might be the starting point.(Fig. -1) Initial Procedure and Observation: Bifrontal External Ventricular Drains (EVD) were placed immediately. The Right EVD had an opening pressure above 40cm and the cerebrospinal fluid (CSF) was clear. On the left side a few drops of fresh blood was the only yield. Post procedure CT scan confirmed accurate placement of catheters, but now with a slight midline shift to the right. Within the next two hours the GCS slowly improved to 10 (E-3, V-2, M-5). But, this did not last for more than eight hours and dropped to 6 again. No fibrinolytic agents were available. Therefore, at this point (within 24hours from the initial bleed) a more aggressive intervention was planned. Surgical Planning: Since the imaging showed signs consistent with increased intracranial pressure from the initial scan, it was decided that a decompressive craniectomy should accompany any other procedure. This time a CT scan was performed with stealth protocol and a stereotaxy assisted procedure was planned. As the patient was left handed, operating on the ipsilateral brain could be considered relatively safe although this is not always true. The target was the occipital horn. It was felt that removal of a well formed hematoma from the all three horns (frontal, temporal, occipital) of the lateral ventricle would be easier from this location. Therefore, a cortical entry site was selected roughly over the parieto-occipital junction. The trajectory was about 45 degrees to the horizontal plane. Operative Details: The left frontal EVD was removed and its entry site was incorporated to the skin incision and to the margin of the bone flap. A left sided wide fronto-temporo-parietal skin flap and a craniotomy flap covering a similar extent was made. The dura was tight; it was opened in a cruciate manner. Then the brain bulged about 1 cm in to the opening. Allowance was made for this change in the trajectory. A 1.5 cm cortical window was made at the calculated entry point. A tunnel of same diameter was dissected down to the target under stealth guidance, using only the suction cannula and the bipolar cautery. On entering the occipital horn there was a gush of CSF under enormous pressure (this indicated that the CSF in the left occipital horn and the temporal horn was entrapped by the hematoma mass that occupied the frontal horn and was not relieved by the standard placement of the EVD in the frontal horn). Then the attention was directed to remove the well formed IVH. Plain suction did not help the evacuation initially. Therefore, a small tumor holding forceps was used to crush the hematoma and these small pieces were sucked out. Later even some large clots could be easily pulled out, too. As anticipated it was much easier to pull out a temporal horn and a frontal horn clot from a occipital horn location. Once the clots were removed an inspection of the lateral ventricle was attempted. With gentle, slightly outward traction using a malleable soft retractor one could visualize most of the temporal horn through the entry tunnel. This confirmed that the temporal horn was clear of any clots. For the frontal horn, same visualization was not possible beyond the upper surface of the thalamus. Although the microscope was on stand-by the need for its use never arose. As soon as the CSF and the IVH was removed the brain sank in to the cranial cavity making the bone flap exclusion highly unnecessary. A ventricular catheter was introduced through the cortical opening to the occipital horn and was directed to the temporal horn and was left at that location. The dural flaps were brought back to the center but was not sutured. A Duragen layer was placed on top of the dura. The bone flap was replaced. Skin and galea was closed in the usual manner. The entire surgical procedure took 98 minutes. Case 2: A right handed hypertensive 63 years old male who has defaulted treatment for several months suddenly became unconscious at home around 10 pm. He was rushed to the local hospital where he was intubated and was transferred to a major neurosurgical center. The CT scan of the head revealed a significant large intracranial hematoma. Due to the low GCS it was decided that non operative management should be carried out and the extremly poor prognosis was notified to the family. The family insisted that maximum possible surgical intervention be done to the patient and the patient was transferred to our center at their request. By this time about 10 hours has elapsed from the initial event.
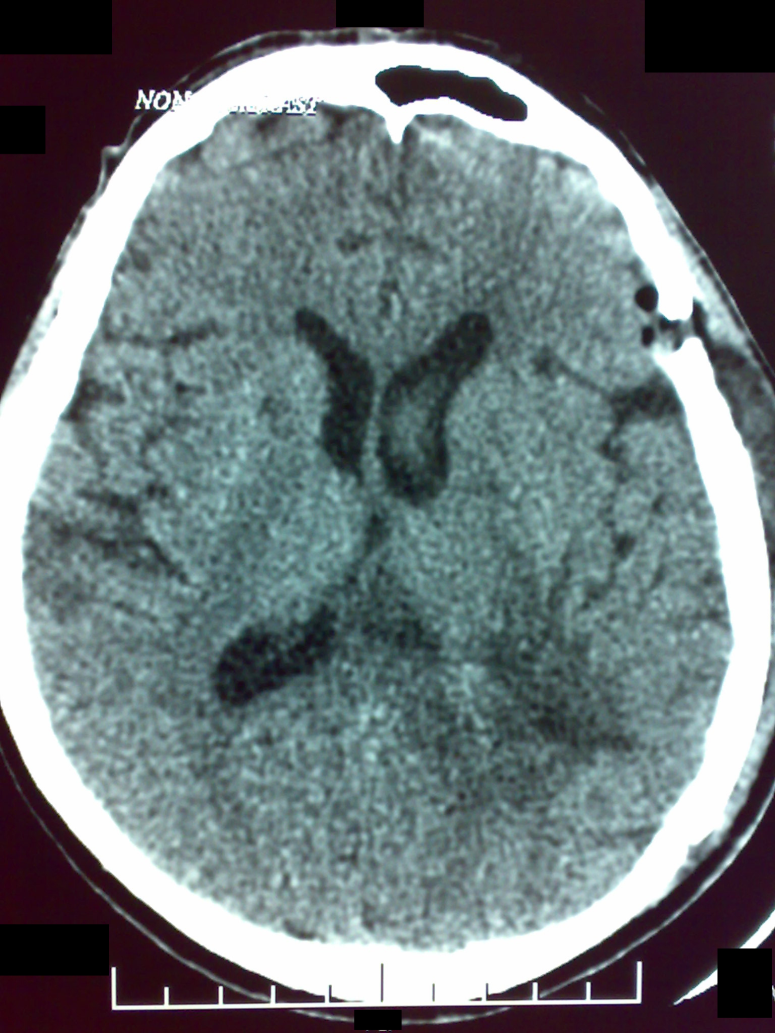
Emergency Room Findings: On arrival in our ER he was intubated and ventilated; had a blood pressure of 240/110. Pupils were 5(right)/3(left) (slow reacting on both sides). His GCS was 5T (E-1, V-T, M-4). There was a left sided hemiparesis. The initial CT scan which was performed in the other center demonstrated a significant IVH involving right temporal and occipital horns with an obstructive hydrocephalus. Right frontal horn did not have any blood, but was compressed. No ICH could be demonstrated.(Fig. -1) Surgical Planning: This was same as the previous case. The difference was that it was on right side. Since there was no frontal horn involvement it was anticipated that the duration of the procedure would be shorter. As immediate surgical evacuation was planned no attempt was made for EVD placement. Operative Details: Right fronto-parieto-temporal skin flap was developed. Fronto-parieto-temporal free bone flap was raised. The tight dura was opened in a cruciate manner. The brain bulged in to the wound. An entry was made at the junction of parieto-occipital cortex. Using a trajectory that was around 45 degrees to the horizontal plane a 1.5 cm tunnel was carved to the right occipital horn. Again CSF emitted under high pressure. A well formed IVH was visible. It was evacuated as before. The brain collapsed to the cranial cavity at this point. At the end the right temporal horn could be visualized by the light traction method that was described in case 1. An EVD catheter was placed in the right temporal horn. The dural flaps were brought back to the original configuration, but not sutured. A Duragen layer was placed over the dura. Bone was replaced and the galea and skin was closed in the usual manner. The entire surgical procedure took 82 minutes. The observations in these cases were made by the treating surgeons. Figure 1: Case 1 - Pre-operative image
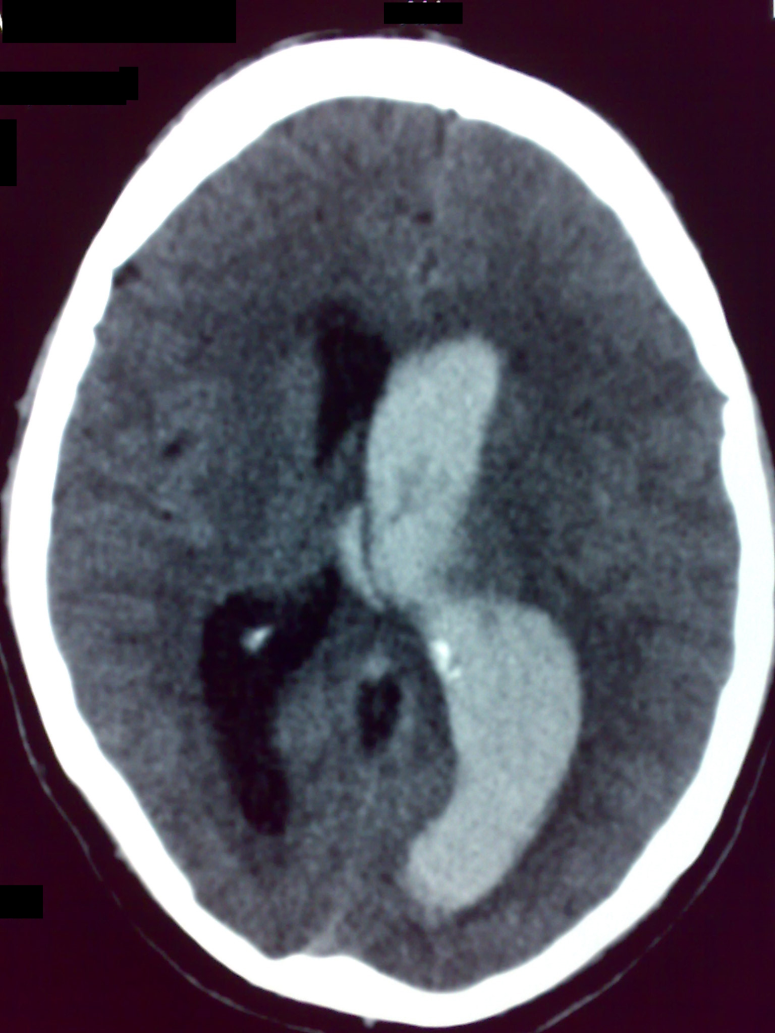 |
| Massive IVH involving left lateral ventricle. The mass effect causes a small midline shift and compresses the 3rd ventricle leading to obstructive hydrocephalus. Tiny ICH noted in the area of thalamus. The sulci are effaced on the affected side. |
Figure 3: Case 2 - Pre-operative image
 |
| IVH does not involve the right frontal horn. No identifiable ICH. There is a significant mass effect and a midline shift. |
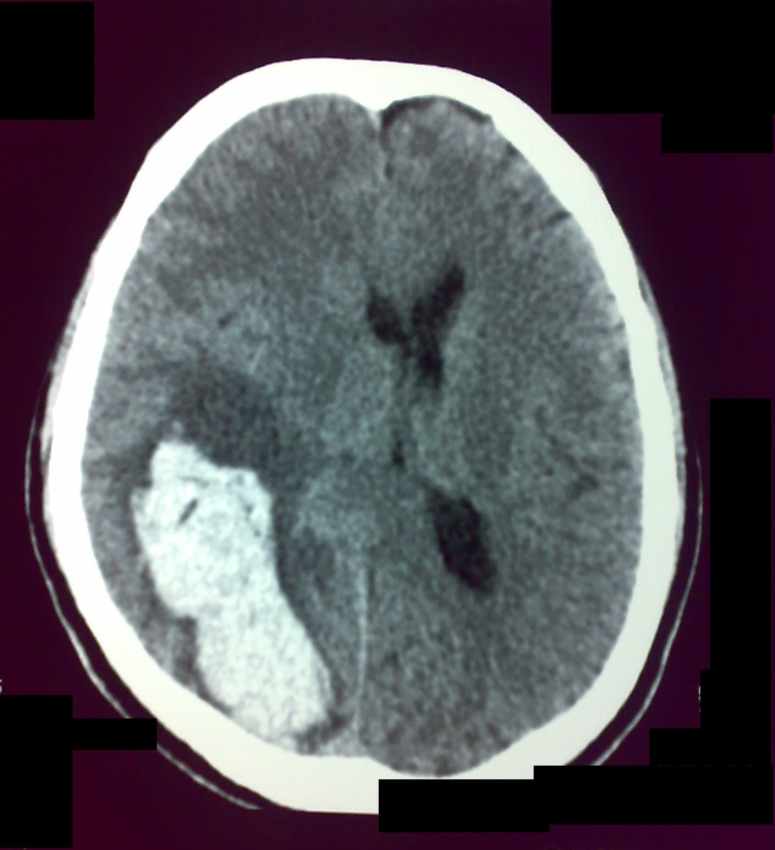
Case 1: The patient was extubated on the first post operative day. He was GCS 13 (E-4, V-3, M-6). The right extremities demonstrated a power of grade 3 and the left grade 5. The post operative scan showed a good clearance of IVH. The left temporal EVD drained cloudy CSF for 3 days. The right frontal EVD drained cloudy CSF for 24 hours then became clear. The ICP remained below 10cm. By the 10th day the power of right extremities were grade 5. It took 18 days for the speech to be perfect. He was discharged from the hospital on the 22nd day after a follow-up CT scan (Fig. -1) . He was GCS 15 and was neurologically intact. Six weeks after the surgery he was able to take an international flight of 10 hours duration to attend to some family business. Case 2: The patient was extubated on the first post operative day. He was GCS 15. However, the left side motor power was grade 3. The right temporal EVD drained cloudy CSF for 48 hours and then got cleared. The post operative scan that was taken prior to removal of the EVD showed satisfactory results(Fig. -1) . Left extremity power improved to grade 5 by the 7th post operative day. On 10th day a follow-up CT scan was taken and the patient was discharged home. By the 4th week he resumed his work as a manager of a pharmaceutical store. Figure 2: Case 1 - Post-operative image
 |
| IVH is completely evacuated.The mass effect is almost eliminated and the sulci on the affected side is visible. A part of post-operative edema is still visible. |
Figure 4: Case 2 - Post-operative image
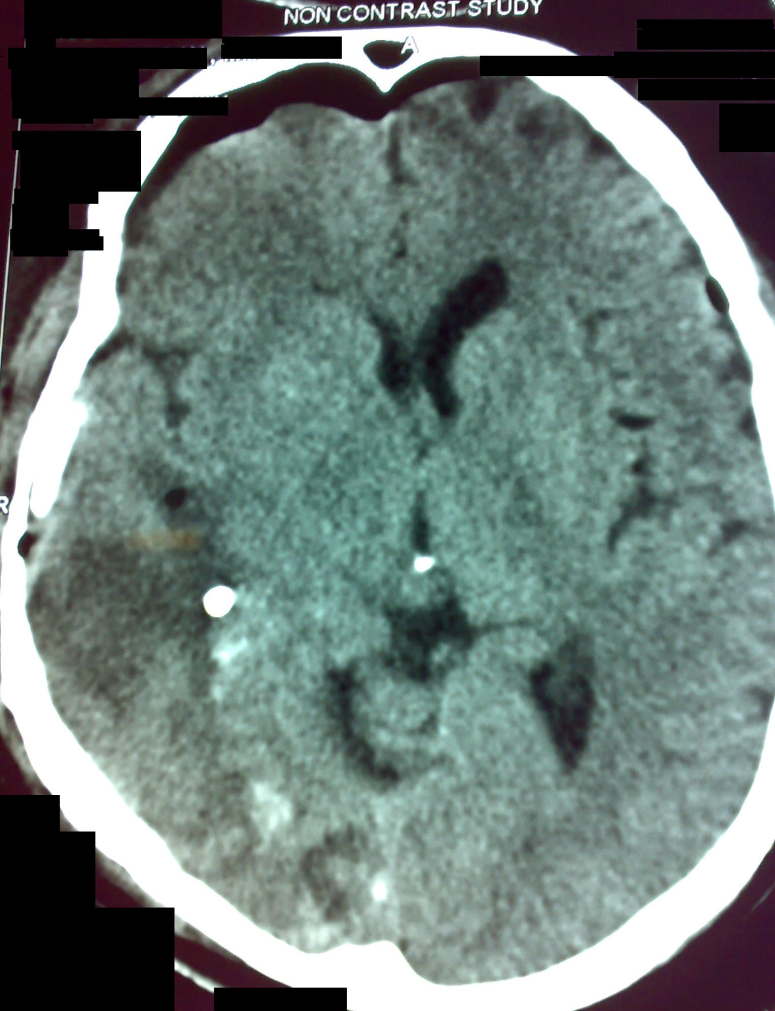 |
| Post-operative image demonstrating adequate decompression. The EVD placed in the right temporal horn is visible in this window. |
Intraventricular extension of a hypertensive ICH is recognized as a bad prognostic factor. Various criteria are developed to assess the out come in such patients4,6 ,5 2,10 . Clinicians have been using several methods to evacuate an IVH. They included catheter drainage (with or without lytic agents) and endoscopic evacuation1,9 . Most of these methods are associated with stereotaxy. Opening into the ventricular system through a conventional craniotomy was considered to cause more harm than good (although this method was used in ruptured aneurysms or AVMs with hematoma extension to ventricles, where primary intervention needed a craniotomy) 8. However, in almost all cases the intraventricular extension has been associated with sizable ICH. In the two cases discussed here, the ICH component is almost negligible in the CT scan. It was the IVH that was causing the obstructive hydrocephalus and the mass effect. Therefore, evacuation of the IVH relieved those effects. And the interventions were performed within 24 hours from the initial bleed. This would have helped in minimizing and deleterious effects of the blood products which were inside the ventricle. The length of entire surgery was around one and a half hour. If fibrinolytic agents were used through an EVD it would have taken much longer to evacuate a large hematoma which is located in the a lateral ventricle. Since the brain parenchymal damage was minimal from any existing small intraparenchymal hematoma, removal of the IVH itself would have reversed the situation. The other advantage of this method was that the procedure was ready for a decompressive craniotomy (although it was not required in these two cases). Although in the first case the thalamus would have been the initial site of bleeding, this is unlikely in the second case. Since the IVH was confined to the temporal and occipital horns, one might consider a choroidal artery origin or a hippocampus origin. This is reported in the literature3 . However, in this case scenario there was no comparison with another IVH evacuation method. There was no comparison with any GCS 6 patient who was not operated. And in these two patients the IVH was involving only a single lateral ventricle. Therefore, a structured case study which compares the above criteria is needed for further evaluation of this method. This is a case report consisting of two patients who presented with hypertensive intraventricular hematomas. Despite their low GCS these patients were managed aggressively with image-guided craniotomy and evacuation of hematomas. The intervention was carried out within 24 hours of the onset of the hemorrhage. Ventricular decompression and removal of clot led to full recovery. Authors concluded that even at a low Glasgow Coma Score of 6, an intervention within 24 hours might lead to an excellent out come in hypertensive unilateral IVH, where the ICH is small. A conventional craniotomy might be helpful in certain cases. The Author(s) wish to thank:
The Nursing Staff of The Central Hospital,
The Nursing Staff of New Nawaloka Hospital,
Dr. Chrishantha Mendis,MD,
Dr. A.T. Alibhoy,MDProject Roles:
1. Chen, H.,Chuang, C.,Tzaan, W.,Hsu, P., Application of neuroendoscopy in the treatment of obstructive hydrocephalus secondary to hypertensive intraventricular hemorrhage. Neurol India 59(6): 861 - 866, 2011 Nov-Dec2. Fortes Lima, T.,Prandini, M.,Gallo, P.,Cavelheiro, S., Prognostic Value of Intraventricular Bleeding in Spontaneous Intraparenchymal Cerebral Hemorrhage of Small Volume: A Prospective Cohort Study. Neurosurgery 11: - , 2011 October3. Furuse, M.,Kuroda, K.,Saura, R.,Kuroiwa, T., A case of hypertensive intraventricular hemorrhage bled from the hippocampus. Neurol Sci 18: - , 2011 August4. Hallevi, H.,Dar, N.,Barreto, A.,Morales, M.,Martin-Schild, S.,Abraham, A., The IVH Score: A novel tool for estimating intraventricular hemorrhage volume: Clinical and research implications. Crit Care Med. 37(7): 969 - , 2009 March5. Hwang, B.,Bruce, S.,Appleboom, G.,Piazza, M.,Carpenter, A.,Gigante, P., Evaluation of intraventricular hemorrhageassessment methods for predicting outcome following intracerebral hemorrhage. J Neurosurgery 14: - , 2011 October6. Nishikawa, T.,Ueba, T.,Kajiwara, M.,Miyamatsu, N.,Yamashita, K., A priority treatment of the intraventricular hemorrhage (IVH) should be performed in the patients suffering intracerebral hemorrhage with large IVH. Clinical Neurology and Neurosurgery 111: 450 - 453, 20097. Rajendra, T.,Kumar, K.,Liang, L., Hypertensive primary intraventricular hemorrhage due to a phaeochromocytoma. Anz J Surg 76(7): 664 - 667, 2006 July8. Rosen, D.,Macdonald, R.,Huo, D.,Goldenberg, F.,Novakovic, R.,Frank, J., Intraventricular hemorrhage from ruptured aneurysm:clinical characteristics, complications, and outcomes in a large, prospective, multicenter study population. J Neurosurgery 107: 261 - 265, 20079. Staykov, D.,Huttner, H .,Lunkenheimer, J.,Volbers, B.,Stuffert, T.,Doerfler, A., Single versus bilateral external ventricular drainage for intraventricular fibrinolysis in severe ventricular haemorrhage. J. Neurol Neurosurg Psychiatry 81: 105 - 108, 201010. Yadav, R.,Mukerji, G.,Shenoy, R.,Basoor, A.,Jain, G.,Nelson, A., Endoscopic Management of Hypertensive IVH with Obstructive Hydrocephalus. BMC Neurology 7(1): - , 2007 January
|

